Knee Replacement Rehab
The knee is the most commonly replaced joint in the body. The decision to have knee replacement surgery is one that you should make in consultation with your orthopedic surgeon and your physical therapist. Usually, total knee replacement (TKR) surgery is performed when people have:
- Knee joint damage due to osteoarthritis, rheumatoid arthritis, other bone diseases, or fracture
- Knee pain or alignment problems in the leg that cause difficulty with walking, performing daily activities, or life tasks
What is total knee replacement (TKR)?
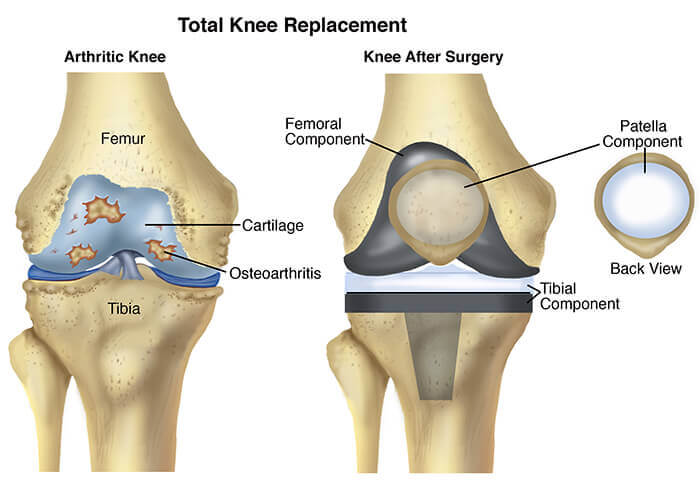
A total knee replacement (TKR) involves removing the ends of the bones at the knee joint (the tibia, sometimes called “shin bone”) and the femur (thigh bone) and replacing them with artificial parts. Replacement parts consist of a metal cap placed on the end of the femur and a plastic cap placed on the top of the shin bone. Sometimes, a plastic insert is used to replace the kneecap.
How can physical therapist help?
Your physical therapist can help ensure that your TKR will be successful by providing evaluation and treatment before and after surgery.
How can a physical therapist help before & after surgery?
Before Your Surgery (“Pre-op Conditioning”)
The better physical shape you are in before TKR surgery, the better your results will be (especially in the short term). Before surgery, your physical therapist will teach you exercises and show you how you will walk with assistance after your operation. Your physical therapist also will discuss precautions and home adaptations, such as removing loose rugs or strategically placing a chair so that you can sit instead of squatting to get something out of a low cabinet. It’s always easier to make these modifications before you have TKR surgery.
If you smoke, quit! That may help improve your healing after surgery. If you are overweight, focus on weight loss prior to surgery. Losing excess body weight may help you recover more quickly, and help improve your function and overall results following surgery.
Immediately Following Your Surgery
With a TKR, you likely will stay in the hospital 2 or 3 days following your surgery. If you have other medical conditions, such as diabetes or heart disease, you might need to stay an additional few days. If you are like most patients, you will be told to put as much weight as comfortable, when standing, on the leg that had surgery. While you are in the hospital, a physical therapist will:
- Show you how to practice walking with a walker or crutches
- Teach you how to safely get in and out of bed or a chair
- Help you continue to do the flexibility and strengthening exercises that you learned before your surgery
During this period, it’s especially important to control the swelling in your knee and to help your incision heal. Your physical therapist may perform electrical stimulation, where electrodes are placed on the skin to stimulate the nerves around the knee to help reduce pain and swelling and promote healing.
Your physical therapist also may apply cold to the knee to help decrease swelling and may recommend that you wear support stockings.
As You Begin to Recover
Proper rehabilitation after a TKR is essential to your recovery. Your physical therapist will help you regain much of your knee range of motion as soon as possible. At this point, you might be walking with a cane or with one crutch.
Your physical therapist can speed up (or “hasten”) your return to activity and help make your new knee better than the old one! Your therapist will tailor range-of-motion exercises, progressive muscle-strengthening exercises, body awareness and balance training, and activity-specific training to your specific needs.
Occasional swelling of the knee joint and lower leg can occur for up to 3 months after surgery. To relieve swelling, you can wear support stockings, apply a cold pack, and elevate your lower leg on a pillow when sitting or lying down.
Range-of-motion exercises. Swelling and pain can make you move your knee less. Your physical therapist can teach you safe and effective exercises to restore the range of motion to your knee so that you can perform your daily activities.
Strengthening exercises. Weakness of the muscles of the thigh and lower leg could make you need to use a cane when walking. Your physical therapist can determine which strengthening exercises are right for you, with the goal of no longer needing to use a cane to walk.
Body awareness and balance training. Specialized training exercises help your muscles “learn” to respond to changes in your world, such as uneven sidewalks or rocky ground. When you are able to put your full weight on your knee without pain, your physical therapist may add agility exercises (exercises that have you practice making quick stops and starts, turns, and changes in direction) and activities using a balance board that challenge your balance and knee control. Your program will be based on the physical therapist’s examination of your knee, on your goals, and on your activity level and general health.
Functional training. When you can walk freely without pain, your physical therapist may begin to add activities that you were doing before your knee pain started to limit you. These might include community-based actions such as crossing a busy street or getting on and off an escalator. Your program will be based on the physical therapist’s examination of your knee, on your goals, and on your activity level and general health.
The timeline for returning to leisure or sports activities varies from person to person; your therapist will be able to estimate yours based on your specific condition.
Activity-specific training. Depending on the requirements of your job or the type of sports you play, you might need additional rehabilitation that is tailored to your job activities (such as climbing a ladder) or sport activities (such as swinging a golf club) and the demands that they place on your knee. A physical therapist can develop a rehabilitation program that takes all of these demands into account.
For more Information, Contact iMotion Physical Therapy today at Fremont, Los Gatos & San Jose, CA Centers.


